Is Our Ground Meat Safe to Eat?
CR tested 351 packages of ground meat and found dangerous bacteria in almost a third of the chicken samples we bought, deadly bacteria in ground beef, and worrisome gaps in the way meat is regulated in this country

Americans love meat—especially ground meat.
We shape it into burgers, meatballs, and meatloaf; stir it into chili and pasta sauce; and stuff it into peppers, lasagna, and tacos. Americans like it so much that in 2021 alone, we purchased more than $13 billion worth of ground beef, turkey, pork, and chicken.
But our love of ground meat comes at a price: It’s a leading cause of food poisoning. Since 2018, 11 outbreaks of illness have been traced back to raw meat, sickening a reported 1,264 people—and at least eight of them involved ground meat, according to the Centers for Disease Control and Prevention.
To assess the current state of the nation’s ground meat supply, Consumer Reports recently tested 351 packages of ground beef, pork, chicken, and turkey purchased at stores throughout the country. (Read more about how we tested (PDF).) What we found was alarming.
Special Report: Lead and Cadmium Could Be in Your Dark Chocolate
CR found dangerous heavy metals in chocolate from Hershey’s, Theo, Trader Joe’s, and other popular brands.
Risky Stuff
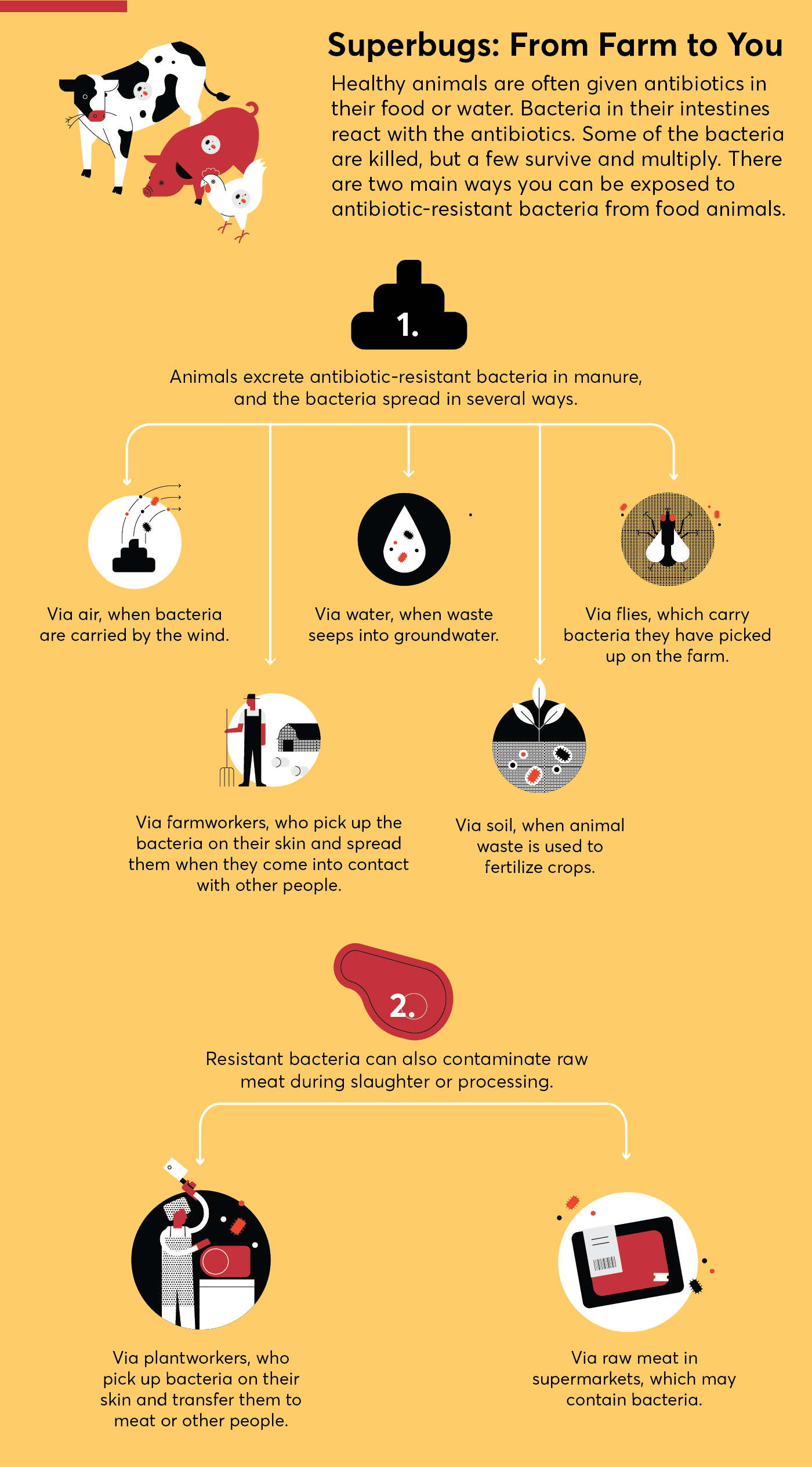
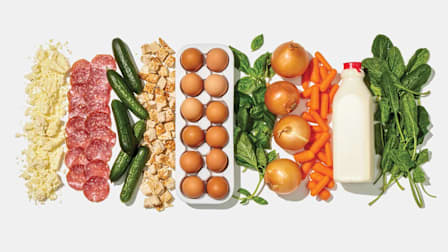
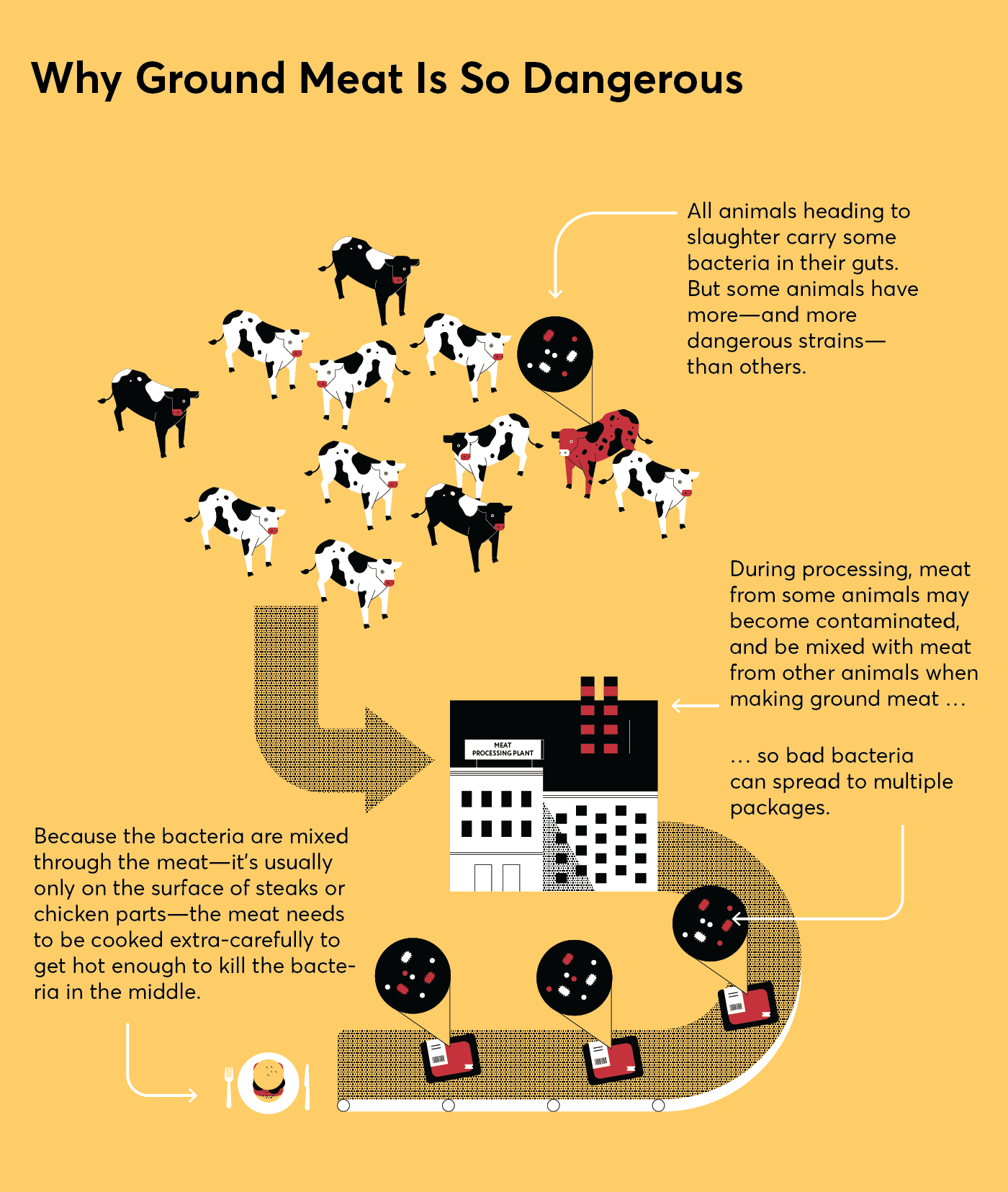
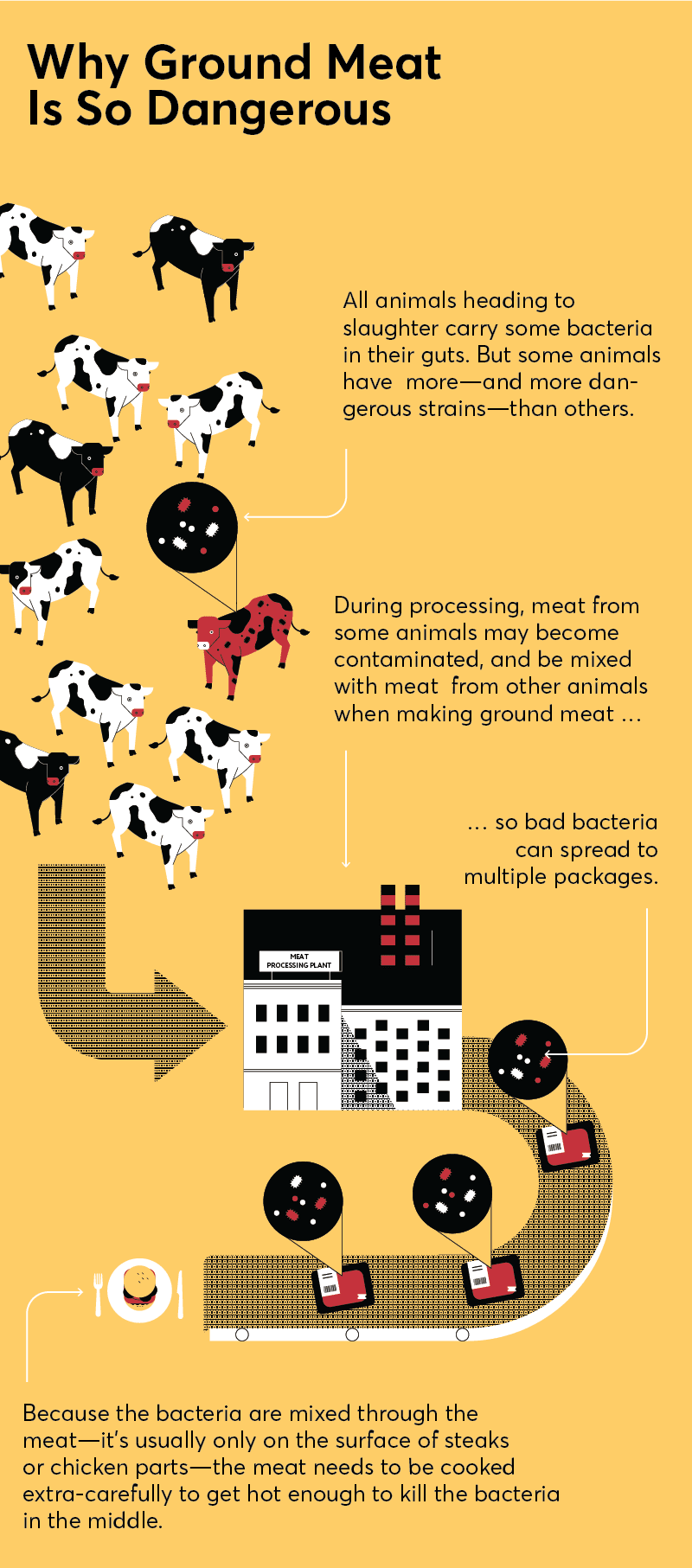
Ground meat is more likely than whole cuts, such as steaks and chicken breasts, to make you sick for several reasons.
It starts at the processing plant, where the meat from multiple animals is ground together. “Even if the meat from just one animal is contaminated with harmful bacteria, such as E. coli or salmonella, it potentially can get distributed into many, many pounds of ground meat,” Rogers says.
Plus, when a steak or chicken breast is contaminated, the bacteria are usually on the surface, where they can be easily killed when cooked. But in ground meat the bacteria get mixed throughout. Serve up a medium-rare burger or an undercooked chicken meatball and you may put people at risk of becoming seriously ill.
In addition, as you make a patty or roll a meatball, “you may handle ground meat more than a whole cut,” Rogers says. “So there are more opportunities for bacteria to spread from your hands and prep surfaces to other foods."
E. Coli in Beef
CR’s finding of E. coli in a package of Kroger-branded ground beef purchased at a grocery store in Seattle triggered a rapid recall of products sold at several chains across the West and Southwest. The action happened so quickly for one main reason: The particular strain CR found—E. coli O157:H7—is one that the USDA takes very seriously.
That’s because it produces a toxin, called shiga toxin, that can harm the intestines, often causing painful, bloody diarrhea and, in 5 to 10 percent of cases, potentially fatal kidney damage.
The USDA has taken an aggressive approach toward that strain of E. coli in ground beef since the 1990s, after a notorious outbreak linked to undercooked hamburgers at Jack in the Box restaurants. More than 600 people became ill, and four children died, prompting the agency to declare O157:H7 and, later, six related strains of shiga toxin-producing E. coli as adulterants. As a result, ground beef (or products that contain it) with those bacteria cannot be legally sold, and manufacturers must recall meat that could be contaminated, even if no illnesses are clearly linked to it.
As CR’s tests found, dangerous E. coli strains still do sometimes show up in ground beef. The recall this year prompted by our tests was one of 23 such recalls since 2018. And some people—about 265,000 a year—continue to be sickened by the strains.
Still, the agency’s aggressive approach has helped, says Bill Marler, a Seattle attorney who focuses on food safety cases and represented consumers sickened in the Jack in the Box outbreak. Faced with the expense and bad publicity that comes with recalls, he says, ground meat producers invested heavily in improved testing and production methods.
“The result is that E. coli O157 cases essentially were cut in half,” he says.
Salmonella in Chicken
While the USDA has taken a hard stance on shiga toxin-producing E. coli in ground beef, that’s not the case for salmonella in chicken or turkey.
“That’s problematic,” says Brian Ronholm, director of food policy at CR. “The agency needs to treat those bacteria, especially in chicken, with a far greater sense of urgency.”
Salmonella is widespread in chickens, in part because of the often crowded and filthy conditions in which they are raised. Nearly 1.35 million people get sick from the bacteria every year, about five times as many as with harmful E. coli. About a fifth of those come from chicken and turkey, including ground versions.
Reducing those numbers has been a stated public health goal for more than a decade. Yet “the large number of people sickened by salmonella hasn’t changed in years,” says Mitzi Baum, CEO at Stop Foodborne Illness, a food safety advocacy group.
And the USDA, far from declaring zero tolerance for the bacteria, actually allows poultry producers to sell meat that may be contaminated with the bacteria. The agency does require poultry processors to regularly test for salmonella. But a plant is allowed to have salmonella in up to 9.8 percent of whole birds it tests, 15.4 percent of parts, and 25 percent of ground chicken. And if producers exceed those levels, they are only given what amounts to a warning, not told to stop selling the meat.

Photo: The Kaplans Photo: The Kaplans
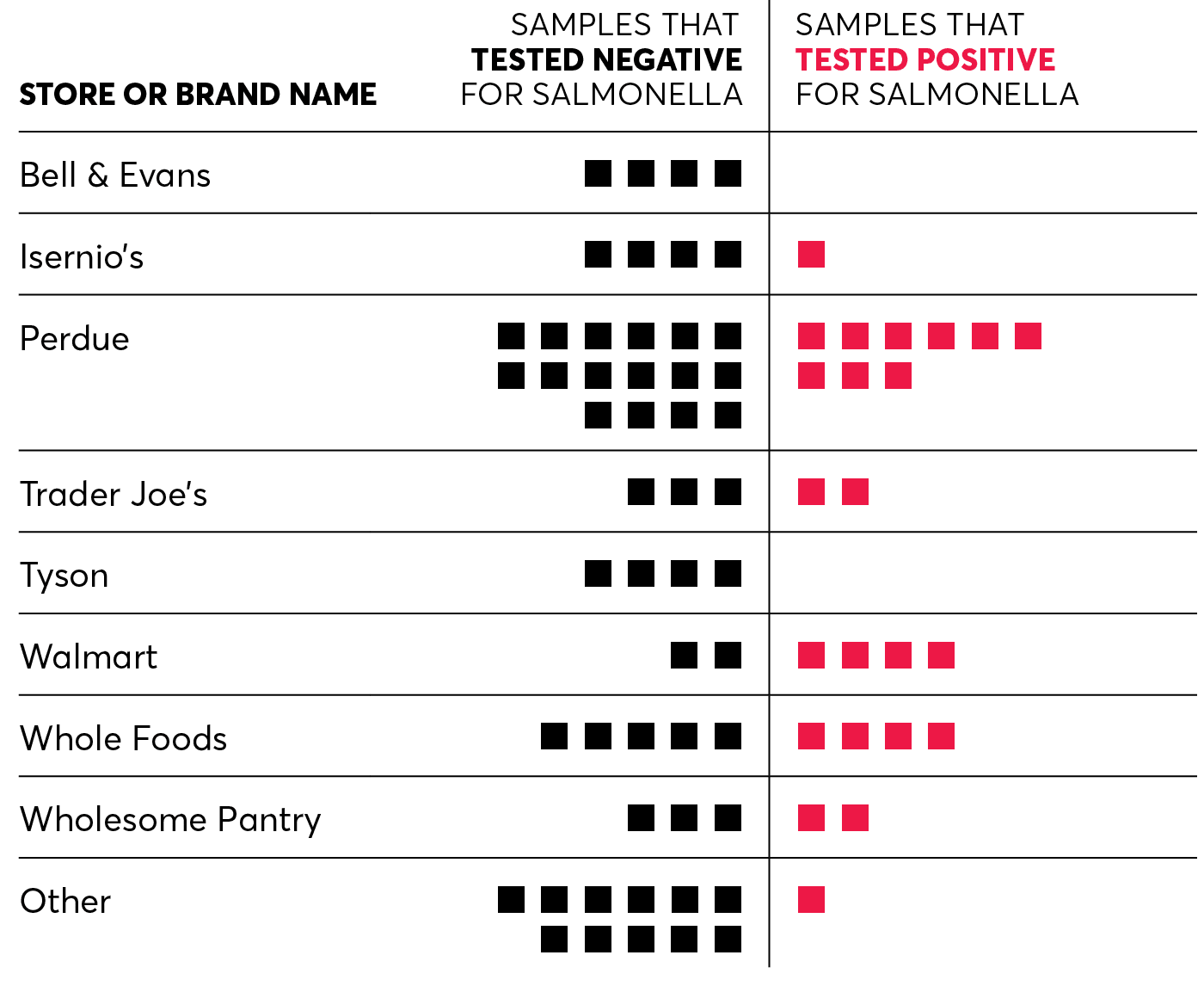
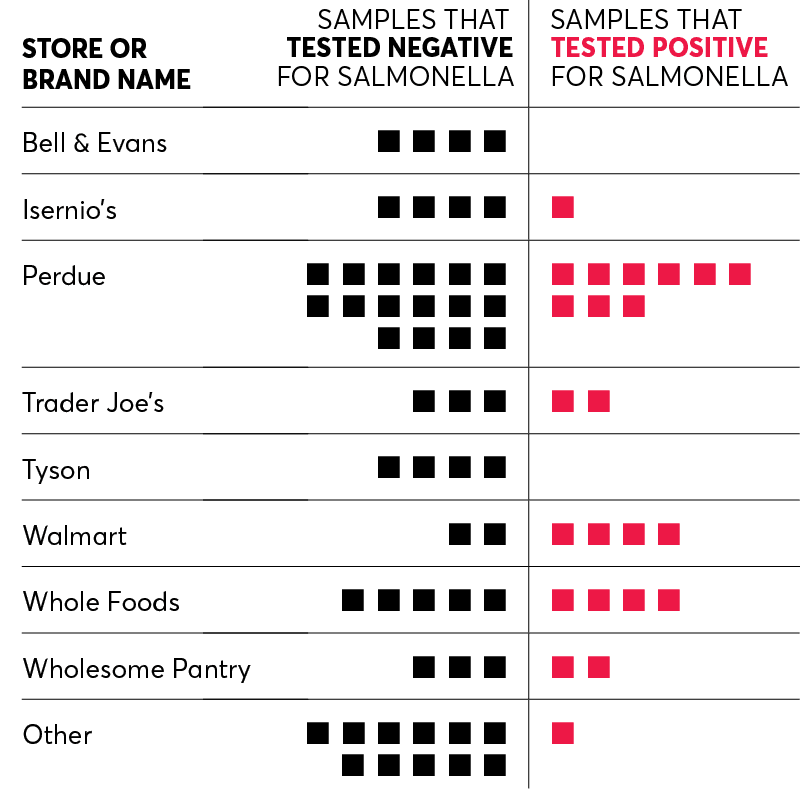
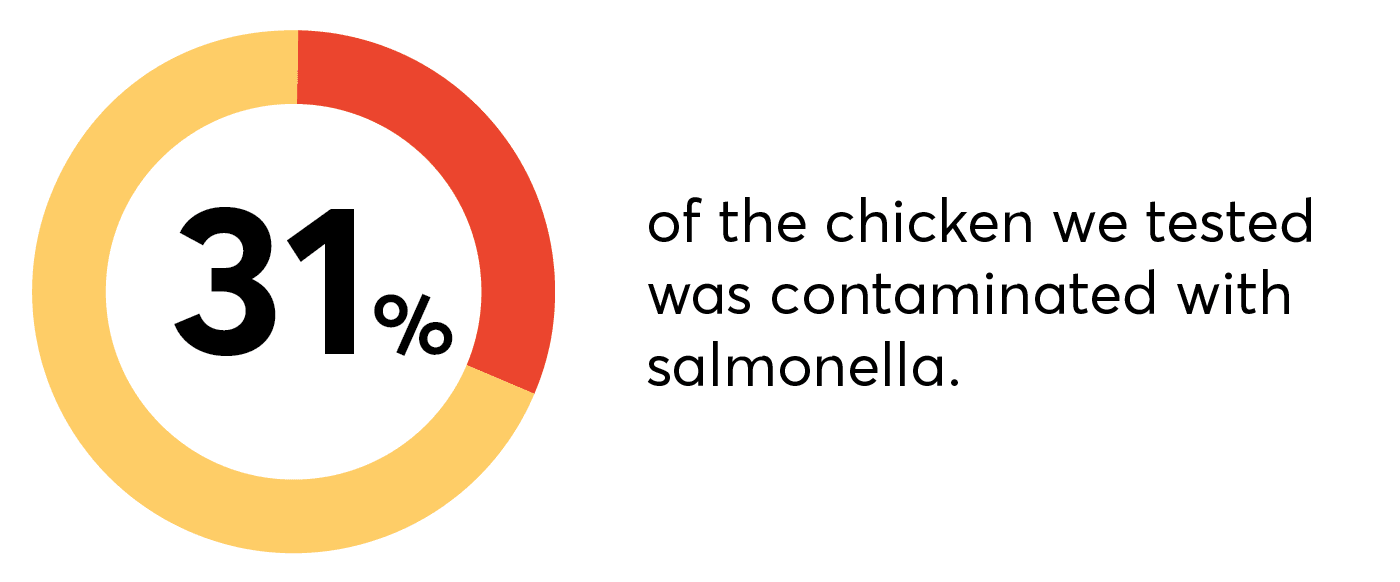
CR found salmonella in 23 of the 75 samples we tested [PDF]—almost a third of them. Nine of the 25 products from Perdue, a leading producer of ground chicken with the most samples in our tests, had salmonella. Samples from Trader Joe’s and Wholesome Pantry, which source their ground chicken from Perdue, also had positive samples, as did some from Isernio’s, Walmart, and Whole Foods.
Overall, no single brand stood out as being statistically better or worse than another. There was even no difference between ground meat from organic chicken and meat from conventionally raised birds.
“The message: Salmonella in ground chicken is more common than it should be,” says Rogers at CR. “This is not an isolated or contained problem."
Legal but Dangerous
If salmonella in chicken is so dangerous and so common, why doesn’t the USDA treat it as aggressively as it does shiga toxin-producing E. coli?
For one thing, lawsuits brought by the meat industry have made it hard for the agency to declare salmonella an adulterant. And the argument—which courts have upheld—surprisingly centers on how Americans like their beef and chicken cooked.
Salmonella in ground chicken is more common than it should be. This is not an isolated or contained problem.
Director of food safety research and testing at Consumer Reports
Congress has said that substances can be considered adulterants in food only if they would “ordinarily” cause a person injury. The courts have determined that it is perfectly ordinary for people to eat beef on the rare side, below the temperature that kills all the E. coli—which means any of the bacteria in the meat are adulterants. By contrast, it is not typical to eat undercooked chicken. So in theory, anyway, salmonella would ordinarily be killed before people eat it. That may be why salmonella is not considered an adulterant in chicken.
But that reasoning is flawed, Baum says, and puts the onus on people to handle chicken with extreme care in their kitchens, not on producers to safely raise and package meat. “It makes the consumer the last safety check in the food,” she says, “and that is an unknown risk for the consumer."
Fixing a Broken System
CR shared our ground chicken test results with all the producers who had at least one sample test positive for salmonella, and asked what steps they take to reduce salmonella contamination.
Perdue, which has partnered with CR and other food safety groups to push for a more rigorous approach to ensuring meat safety, says that in a recent spot check it did of 312 samples, only 17, or 5.4 percent, were positive for salmonella. That’s far lower than the 36 percent of Perdue samples with the bacteria in CR’s tests.
Perdue and several other producers say they are taking steps to reduce salmonella in their products.
Tricia Moriarty, a spokesperson for Walmart, says the company began a “salmonella interventions program” in 2014. “While no system will eliminate all salmonella bacteria, our program has significantly reduced the amount” in the products it gets from suppliers, she says. Whole Foods says that it has a quality assurance team that assesses salmonella reports from the USDA and that “if a processing plant is not meeting our expectations, we investigate to determine root cause and a corrective action plan.” And Wholesome Pantry says the company holds “our suppliers to strict industry standards.”
Tom Super, senior vice president of communications at the National Chicken Council, an industry group, says that such steps have helped improve meat safety and that some risk is inescapable. “Any raw agricultural product, including fresh fruit, vegetables, meat, and poultry, is susceptible to naturally occurring bacteria,” he says. “No legislation or regulation can keep bacteria from existing.”
But independent food safety experts say larger, more systemic changes are needed.
Lance Price, PhD, director of the Antibiotic Resistance Action Center at George Washington University in Washington, D.C., says the best solution would be to reduce the number of chickens that carry salmonella in the first place and for the agency to declare the bacteria to be adulterants. That would require companies to recall any product that tests positive for the bacteria, instead of waiting for outbreaks when people get sick, he says.
But he also acknowledges that such steps are unlikely, at least in the short term. Instead, he, along with CR’s Ronholm and other safety advocates, says the USDA should focus on sharply reducing the percentage of chicken samples allowed to test positive for salmonella.
In addition, the agency should focus on the most problematic strains of salmonella. Last year CR, along with the Center for Science in the Public Interest and other food safety groups, petitioned the USDA, urging it to reduce the salmonella strains that pose the biggest threat to human health. The agency identified three strains to focus on: infantis, typhimurium, and enteritidis.
In CR’s test, 91 percent of the salmonella detected in ground chicken was from those three strains.
The groups also say the USDA needs more authority to inspect facilities that breed and raise poultry and, when a plant is found to have high salmonella rates, to quickly shutter its operations.
Sandra Eskin, deputy undersecretary for food safety at the USDA, says, “The results of Consumer Reports’ sampling project underscores why [the agency] is rethinking our existing strategy so that it is more effective in reducing salmonella infections” from poultry. She says the agency is gathering recommendations from independent food safety experts and working with industry to develop pilot projects “to test-drive different control strategies.”
When it comes to shiga toxin-producing E. coli strains, Ronholm says they should be addressed aggressively wherever they are found. He says that those strains are now considered adulterants only in ground beef and mechanically tenderized beef. (Those are cuts of meat pierced by a machine to make them more tender, a process that can drive bacteria from the surface into the meat.)
@consumerreports Nearly 1/3 of the ground chicken we sampled from across the country tested positive for salmonella. Tell the USDA to reduce salmonella food poisoning: take action at cr.org/groundchickenpetition #foodtok #foodtiktok #salmonella #foodsafety
♬ original sound - Consumer Reports
Handle With Care
Until industry and the government take stronger steps to limit salmonella, E. coli, and other bacteria in meat, the best way to prevent foodborne illness remains practicing scrupulous kitchen hygiene. Here are some tips, from shopping to prep to storing leftovers.
• At the grocery store, keep raw meats in a disposable bag, separated from other foods. This can reduce the chance of a contaminated package coming into contact with other foods, especially uncooked foods that are consumed raw, such as fruits and salads.
• In the fridge, store raw meat in a bag or bowl. That keeps juices from leaking onto other surfaces or foods.
• Don’t rely on how the meat looks or smells. You can’t tell whether meat or poultry contain harmful bacteria. Use ground meat within two days of purchase. Or freeze it, either in its original package or repackaged. Either way, wrap it in foil or plastic wrap, or put it in a freezer bag or an airtight container.
• Thaw frozen meat in the refrigerator. That’s to keep meat cooled to below 40° F as it thaws, a temperature that impedes the growth of bacteria. Setting it out on the counter can accelerate that growth. Once the meat is thawed, use it within a day or two for ground meat or any type of poultry, and within three to five days for cuts of beef or pork.
• Keep burgers chilled. Don’t take the meat out of the refrigerator until you’re ready to make the patties, and then put the patties in the refrigerator until you’re ready to cook them. That helps prevent any bacteria that may be in the meat from multiplying—and can help your patty hold together during cooking. Tip: When forming patties, make a slight indentation in the top of each with your thumb to keep shrinkage to a minimum.
• Don’t rinse raw meat. Doing so is more likely to spread any bacteria around the sink or counter than it is to remove bacteria. If you like, pat the meat with a paper towel first instead.
• When preparing, wash, wash, wash. Wash your hands in hot soapy water before you start prepping, then after every time you touch raw meat, and again when you’re finished. And wash any knives used on meat before cutting other foods.
• Use dedicated cutting boards. That means one for raw meat, and another for fruits and vegetables.
• Get a meat thermometer and use it. You can’t gauge whether meat is fully cooked by how it looks. Instead, check the internal temperature with a thermometer. Ground beef and pork are safe when cooked to 160° F. Poultry—ground, whole, and parts—should be cooked to 165° F; beef roasts and steaks, and pork roasts and chops, to 145° F.
• Refrigerate leftovers promptly. Cooked food shouldn’t be left out longer than 2 hours after it’s removed from the stove, oven, or grill. (One hour is the limit if you’re outside and the temperature is 90° F or higher.)
Editor’s Note: This article also appeared in the August 2022 issue of Consumer Reports magazine.